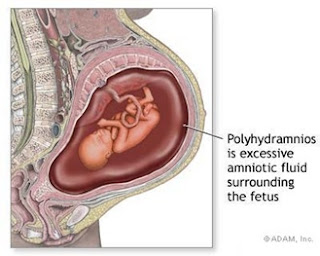
Polyhydramnios
- Abnormally large amount of amniotic fluid in the uterus.
- Normal range from 500 to 1,000 ml at term; typically greater than 2,000 ml in polyhydramnios at 40 weeks’ gestation.
- Possible complications:
- prolapsed umbilical cord when membranes rupture
- increased incidence of malpresentations
- increased perinatal mortality from fetal malformations and premature deliveries
- increased incidence of postpartum maternal hemorrhage
1. Mild Polyhydramnios – when amniotic fluid pockets is between 8 to 11 cm in vertical dimensions. (85%)
2. Moderate Polyhydramnios – when amniotic fluid pockets is between 12 to 15 cm in vertical dimensions. (17%)
Predisposing Factors
- Multiple pregnancy
- Fetal abnormalities – esophageal atresia, anencephaly, spina bifida
- Diabetes Mellitus
Pathophysiology
- Normally, amniotic volume is maintained by a balance of fetal fluid production (lung liquid and urine) and fluid resorption (fetal swallowing and flow across the membrane to the fetus or the maternal uterus).
- Fetal urine is the primary source of amniotic fluid with output at term ranging from 400 to 1,200 ml/day.
- Fetal swallowing is believed to be the major route of amniotic fluidresorption.
- With polyhydramnios, fluid accumulates because of a problem with the fetus’s ability to swallow or absorb the fluid or as a result of over production of urine.
- Fluid may have increased gradually (chronic type) by the third trimester or rapidly (acute type) between 20 and 24 week’s gestation.
Causes
- Exact cause is unknown in about 35% of all cases.
- May be associated with:
- diabetes mellitus (about 25%)
- erythroblastosis ( about 10%)
- multiple gestations (about 10%)
- anomalies of the central nervous system (such as neural tube defects)
- GI anomalies such as tracheoesophageal fistula that prevent ingestion of the amniotic fluid (about 20%).
Assessment Findings
- Depend on the length of gestation, the amount of amniotic fluid, and whether the disorder is chronic or acute.
- Mild signs and symptoms; maternal abdominal discomfort, slight dyspnea, and edema of feet and ankles.
- Severe signs and symptoms; severe dyspnea, orthopnea, and significant edema of the vulva, legs, and abdomen.
- Symptoms common to mild and severe cases: uterine enlargement greater than expected for the length of gestation, and difficulty in outlining the fetal parts and in detecting fetal heart sounds.
Test Results
- Ultrasonography shows evidence of excess amniotic fluid as well as underlying conditions.
- Amniotic fluid index is 20 cm or greater.
Treatment
- High protein, low sodium diet
- Mild sedation
- Indomethacin therapy – a drug that decreases the fetal urine formation. The side effect of indomethacin, as with other prostaglandin synthase inhibitors, is the potential premature closure of the ductus arteriosus.
- Amniotomy – The fluid is removed by a needle inserted through the cervix. The danger of this procedure is cord proplapse and abruptio placenta. to prevent these complications, amniotic fluid must be removed gradually.Watch closely for hemorrhage after delivery, prevent uterine relaxation by massaging the uterus and administering oxytoxin as ordered.
- Induction of labor if the fetus is mature and symptoms are severe.
Nursing Interventions
- Mild to moderate degrees usually does not require treatment.
- Hospitalization if symptoms are severe dyspnea, abdominal pain and difficult ambulation.
- Maintain bed rest with sedation to make the situation endurable.
- Monitor the patient for signs and symptoms of premature labor.
- Monitor maternal vital signs and fetal heart rate frequently; report changes immediately.
- Prepare the patient for amniocentesis and possible labor induction, as appropriate; keep in mind that amniocentesis for fluid removals is only temporary and may need to be done repeatedly.